Chimeric Antigen Receptor (CAR) T cells are genetically engineered T cells that express receptors that recognize specific tumor markers for the treatment of blood cancers. So far, 6 types of CAR T cell therapies have been approved by the United States FDA for the treatment of leukemia, lymphoma, and multiple myeloma; several clinical trials of CAR T cell therapy are ongoing.
However, CAR T cell therapy still has significant limitations, including cytokine release syndrome (CRS), neurotoxicity, antigen escape, and durability of therapeutic effects. Especially in regards to the treatment of solid tumors, due to the influence of factors such as the microenvironment, no major clinical breakthrough has been achieved so far. This article discusses the challenges and progress of CAR T cell therapy in the treatment of solid tumors.
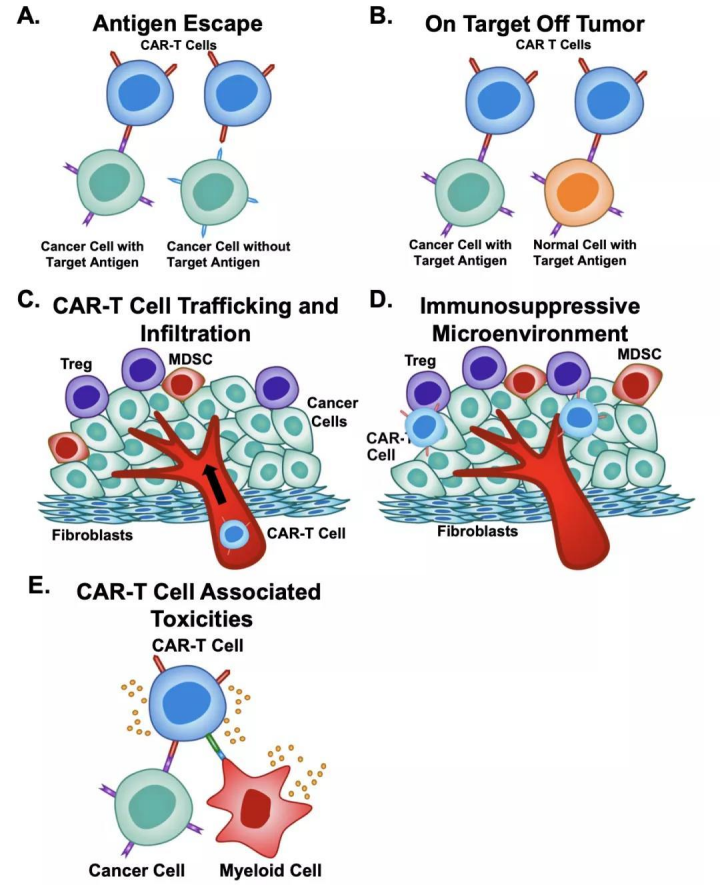
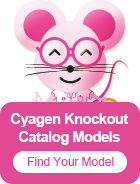
Figure 1. Current challenges in CAR-T cell therapy include[1] (A) antigen escape, (B) on-target off-tumor effects, (C) trafficking and infiltration of tumors, (D) the immunosuppressive tumor microenvironment, and (E) CAR-T cell-associated toxicities.
The principle of CAR T cells killing tumor cells is the following:
1. The extracellular antigen binding domain of the CAR molecule specifically recognizes tumor antigens;
2. The recognition signal is transmitted to the intracellular domain of the CAR molecule;
3. The intracellular domain activates T cells, so that the cells proliferate, synthesize perforin and granzyme, release cytokines, etc., and kill tumor cells.
In order to maximize these functions, the structural design of CAR molecules is crucial.
CAR molecules consists of 4 main components: (1) an extracellular target antigen-binding domain, (2) a hinge region, (3) a transmembrane domain, and (4) one or more intracellular signaling domains.[1]
The antigen binding domain is the portion of the CAR that confers target antigen specificity. The principle is to connect the variable heavy (VH) and light (VL) chains of monoclonal antibodies via a flexible linker to form a single-chain variable fragment (scFv) to specifically recognize tumor surface antigens. [1]
The hinge region is defined as the extracellular structural region that extends from the binding units to the transmembrane domain. The hinge functions to provide flexibility to overcome steric hindrance and contributes to the length in order to allow the antigen-binding domain to access the targeted epitope. [1]
The major function of the transmembrane domain is to anchor the CAR to the T cell membrane[1]. Studies have shown that the transmembrane region may affect the expression level and stability of CAR, and play a role in signal transduction [2][3][4].
The most attention in CAR engineering has been focused on understanding the effects of CAR co-stimulation. The main difference between the first 1-3 generations of CARs comes from the intracellular co-stimulation domain. The two most common and FDA-approved co-stimulatory domains, CD28 and 4-1BB, are highly effective in activating T cells and inducing T cells to perform different functions [5].
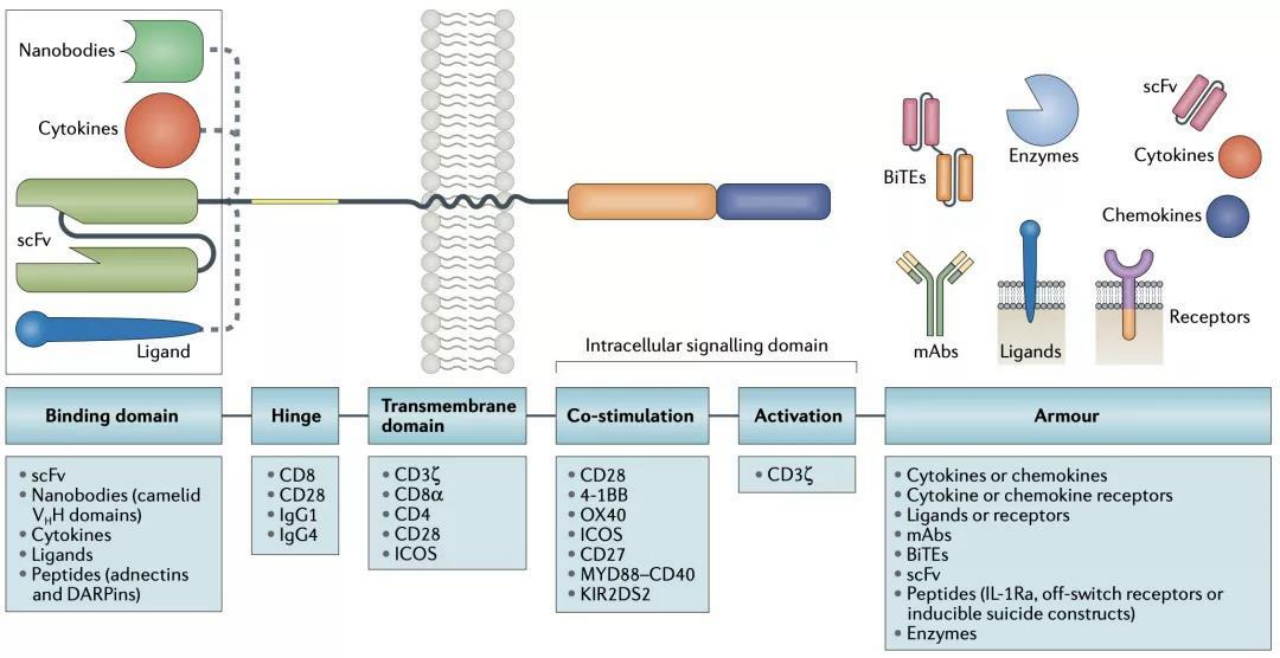
Figure 2. Blueprint of CAR Design[20]
Tumor antigen heterogeneity is one of the barriers to CAR T cell therapy against solid tumors. There are two main types of tumor antigens: tumor-associated antigens (TAAs) and tumor-specific antigens (TSAs). TAA is highly expressed in tumor cells and low in normal tissue cells; TSA is only expressed in tumor cells, not in normal tissue cells, so it is the most ideal antigen target. Due to the extremely difficult discovery and screening of TSA targets, TAAs are the most commonly used targets for CAR identification. The diverse expression of TAAs by different types of tumor cells may affect the identification of cancer cells by CAR T cells, thereby influencing the therapeutic effect.
There are various methods to target CAR T cells to identify multiple tumor-associated antigens, such as co-expression of multiple CARs on a single T cell and programmable CAR expression regulation. Expression of two or more antigen recognition domains allows a single CAR T cell to recognize multiple antigens expressed on tumor cells, thereby eliminating the adverse effects of antigenic heterogeneity.
Figure 3. Immunosuppressive microenvironment in solid tumors [13]. a Effector cells and target cells. b Immunosuppressive cells and cytokines. c Physical barriers. d Intratumoral microenvironment. e Other immunosuppressive factors.
CAR T cells can exist in the blood and lymphatic systems. Therefore, for hematological tumors, CAR T cells have more opportunities to access blood tumor cells[1], while in solid tumors, it is more difficult to penetrate the tumor tissue through the blood system[6]. Furthermore, the lack of expression of chemokines involved in T cell penetration into tumor tissueas well as the presence of dense fibrotic stroma in solid tumors together result in a reduced ability of CAR T cells to migrate and invade cells in solid tumors[7].
Many cases have been reported which use a direct local injection of CAR T cells into tumor sites, such as the brain[8], breast[9], pleura[10], and liver[11]. Local injection of CAR T cells may reduce the risk of off-target effects. However, many solid tumors are metastatic, which is a major difficulty with local injection of CAR T cells. On the other hand, chemokines have been used in some clinical studies to mediate the delivery of CAR T cells to enhance tumor localization. For example, the expression of macrophage colony-stimulating factor 1 receptor (CSF-1R) in CAR T cells makes these cells responsive to CSF-1, a monocyte chemokine that is enriched in many solid tumors. While enhancing the signal transduction of CAR T cell proliferation, it does not affect the lethality and toxicity of cells [12].
The tumor microenvironment of solid tumors promotes tumor growth and proliferation while causing immunosuppression to CAR T cells by modifying parameters such as:
Burga et al.[14] used genetically engineered Gr-1 antibodies to deplete myeloid-derived suppressor cells (MDSCs) to enhance the tumor-killing effect of CAR T in a mouse model. There have also been reports of breaking physical barriers in solid tumors by constructing CAR-T cells that secrete enzymes that degrade the extracellular matrix (ECM)[15].
In recent years, research on solid tumor targets has gradually increased, and a considerable number of them have entered Phase II clinical trials. Some common solid tumor targets and indications are listed in Table 1.
|
Target |
Cancer |
Clinical Phases |
|
Mesothelin |
Ovarian cancer, cervical cancer, pancreatic cancer, lung cancer |
Clinical phase I/II |
|
MUC1 |
Advanced solid tumor, lung cancer |
Clinical phase I/II |
|
Glypican-3 |
Liver cancer |
Clinical phase I |
|
GD2 |
Brain cancer |
Clinical phase I/II |
|
HER2 |
Central nervous system tumors, pediatric glioma, breast cancer |
Clinical phase I/II |
Table 1. Common Targets and Indications for Solid Tumors
(Clinical Data Source: ClinicalTrials.org)
Tumor-associated glycoprotein 72 (TAG72), which is highly expressed on the surface of ovarian tumors, has been used as a target for CAR T cell therapy [16]. The authors of this study constructed a second-generation TAG72-BBζ CAR and showed that regional intraperitoneal delivery of TAG72-BBζ CAR T cells significantly reduced tumor growth and extended overall survival of mice. Studies have also shown that CARs constructed using MUC16 or HER2 have tumor-targeting ability and can inhibit the growth and proliferation of ovarian cancer cells. Mesothelin is a glycoprotein that exists on the cell surface and has been shown to be highly expressed in a variety of cancer cells.
In the treatment of liver cancer, research on CAR T cell therapy has just started. The research on carcinoembryonic antigen (CEA), Glypican-3, mucin-1 and other targets based on CAR T cells has achieved certain results in the treatment of liver cancer. The combination of GPC3 antibody and CAR T-cell therapy may be an effective treatment for hepatic malignant tumors[21].
In the study of lung cancer, the A549 cell line of lung cancer was treated with CAR T cells specific for receptor tyrosine kinase-like orphan receptor 1 (ROR1), which showed strong antitumor activity[18]. Srivastava et al. pretreated with oxaliplatin/cyclophosphamide (Ox/Cy) chemotherapy after finding that ROR1 CAR T cells were poorly infiltrated and dysfunctional. This regimen improves the migration of CAR T cells to the tumor, and combined with anti-PD-L1 checkpoint blockers can improve the survival rate [19]. In addition, other studies have confirmed that CAR T cell-based mesothelin, erythropoietin-producing hepatocyte receptor A2 (EphA2), and PSCA and mucin-1 are also ideal therapeutic targets for lung cancer.
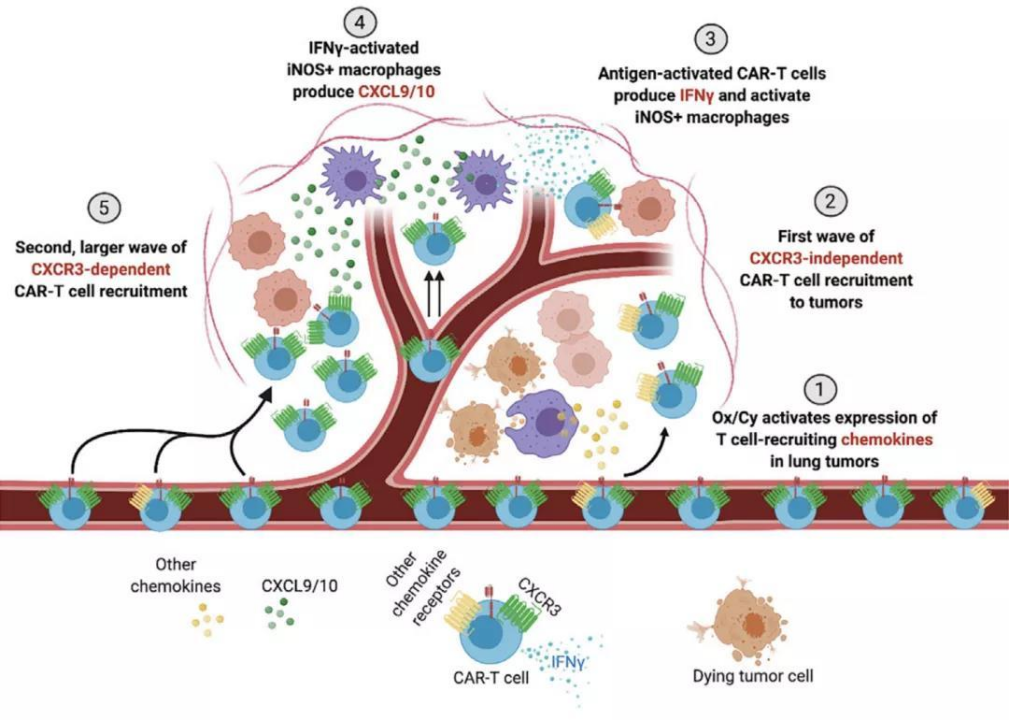
Figure 5. CAR T Cell Therapy Combined with Ox/Cy Chemotherapy Pretreatment[19]
CAR T cell therapy has brought a glimmer of light to patients with hematological tumors, and has a good prospect in the treatment of advanced malignant tumors. However, factors such as immunosuppression, physical barriers, and antigenic heterogeneity in the tumor microenvironment hinder the efficacy of CAR T cells in solid tumors. Researchers have done a lot of forward-looking work to meet these challenges. Novel ideas and creative CAR engineering designs are constantly created and updated. We are also looking forward to the advent of the perfect toolkits to enable CAR T cell therapy of solid tumors.
Due to the particularity of CAR T cell therapy principles, more issues need to be considered in the CAR T development process, such as the selection of therapeutic targets, the distribution of CAR T cells in vivo, and cytotoxicity. Cyagen provides one-stop cell therapy research solutions supporting CAR T and other cell therapy development programs,, including CAR virus preparation, the construction of tumor immune cells and animal models, and the entire process of in vivo/in vitro drug efficacy evaluation — accelerating the development of CAR T and cell therapy research.

|
Viral vector manufacturing |
Construction of the immune model |
In vitro pharmacodynamic evaluation |
In vivo pharmacodynamic evaluation |
|
|
|
|
Request a quote now. Alternatively, you can always email service-apac@cyagen.com to inquire about our services or obtain a quote for your project.
[1] Sterner, R. C., & Sterner, R. M. (2021). CAR T cell therapy: current limitations and potential strategies. Blood Cancer Journal, 11(4), 1-11.
[2] Bridgeman, J. S., Hawkins, R. E., Bagley, S., Blaylock, M., Holland, M., & Gilham, D. E. (2010). The optimal antigen response of chimeric antigen receptors harboring the CD3ζ transmembrane domain is dependent upon incorporation of the receptor into the endogenous TCR/CD3 complex. The Journal of Immunology, 184(12), 6938-6949.
[3] Guedan, S., Posey Jr, A. D., Shaw, C., Wing, A., Da, T., Patel, P. R., ... & June, C. H. (2018). Enhancing CAR T cell persistence through ICOS and 4-1BB costimulation. JCI insight, 3(1).
[4] Zhang, T., Wu, M. R., & Sentman, C. L. (2012). An NKp30-based chimeric antigen receptor promotes T cell effector functions and antitumor efficacy in vivo. The Journal of Immunology, 189(5), 2290-2299.
[5] Kawalekar, O. U., O’Connor, R. S., Fraietta, J. A., Guo, L., McGettigan, S. E., Posey Jr, A. D., ... & June, C. H. (2016). Distinct signaling of coreceptors regulates specific metabolism pathways and impacts memory development in CAR T cells. Immunity, 44(2), 380-390.
[6] Salmon, H., Franciszkiewicz, K., Damotte, D., Dieu-Nosjean, M. C., Validire, P., Trautmann, A., ... & Donnadieu, E. (2012). Matrix architecture defines the preferential localization and migration of T cells into the stroma of human lung tumors. The Journal of clinical investigation, 122(3), 899-910.
[7] Li, J., Li, W., Huang, K., Zhang, Y., Kupfer, G., & Zhao, Q. (2018). Chimeric antigen receptor T cell (CAR T) immunotherapy for solid tumors: lessons learned and strategies for moving forward. Journal of hematology & oncology, 11(1), 1-18.
[8] Brown, C. E., Alizadeh, D., Starr, R., Weng, L., Wagner, J. R., Naranjo, A., ... & Badie, B. (2016). Regression of glioblastoma after chimeric antigen receptor T-cell therapy. New England Journal of Medicine, 375(26), 2561-2569.
[9] Tchou, J., Zhao, Y., Levine, B. L., Zhang, P. J., Davis, M. M., Melenhorst, J. J., ... & June, C. H. (2017). Safety and efficacy of intratumoral injections of chimeric antigen receptor (CAR) T cells in metastatic breast cancer. Cancer immunology research, 5(12), 1152-1161.
[10] G. L., Haas, A. R., Maus, M. V., Torigian, D. A., Soulen, M. C., Plesa, G., ... & June, C. H. (2014). Mesothelin-specific chimeric antigen receptor mRNA-engineered T cells induce antitumor activity in solid malignancies. Cancer immunology research, 2(2), 112-120.
[11] Hardaway, J. C., Prince, E., Arepally, A., & Katz, S. C. (2018). Regional infusion of chimeric antigen receptor T cells to overcome barriers for solid tumor immunotherapy. Journal of vascular and interventional radiology: JVIR, 29(7), 1017-1021.
[12] Lo, A. S. Y., Taylor, J. R., Farzaneh, F., Kemeny, D. M., Dibb, N. J., & Maher, J. (2008). Harnessing the tumour-derived cytokine, CSF-1, to co-stimulate T-cell growth and activation. Molecular immunology, 45(5), 1276-1287.
[13] Zhang, E., Gu, J., & Xu, H. (2018). Prospects for chimeric antigen receptor-modified T cell therapy for solid tumors. Molecular cancer, 17(1), 1-12.
[14] Burga, R. A., Thorn, M., Point, G. R., Guha, P., Nguyen, C. T., Licata, L. A., ... & Katz, S. C. (2015). Liver myeloid-derived suppressor cells expand in response to liver metastases in mice and inhibit the anti-tumor efficacy of anti-CEA CAR T. Cancer Immunology, Immunotherapy, 64(7), 817-829.
[15] Caruana, I., Savoldo, B., Hoyos, V., Weber, G., Liu, H., Kim, E. S., ... & Dotti, G. (2015). Heparanase promotes tumor infiltration and antitumor activity of CAR-redirected T lymphocytes. Nature medicine, 21(5), 524-529.
[16] Murad, J. P., Kozlowska, A. K., Lee, H. J., Ramamurthy, M., Chang, W. C., Yazaki, P., ... & Priceman, S. J. (2018). Effective targeting of TAG72+ peritoneal ovarian tumors via regional delivery of CAR-engineered T cells. Frontiers in immunology, 9, 2268.
[17] Cao, B., Liu, M., Wang, L., Liang, B., Feng, Y., Chen, X., ... & Zhang, Z. (2020). Use of chimeric antigen receptor NK-92 cells to target mesothelin in ovarian cancer. Biochemical and biophysical research communications, 524(1), 96-102.
[18] Wallstabe, L., Göttlich, C., Nelke, L. C., Kühnemundt, J., Schwarz, T., Nerreter, T., ... & Hudecek, M. (2019). ROR1-CAR T cells are effective against lung and breast cancer in advanced microphysiologic 3D tumor models. JCI insight, 4(18).
[19] Srivastava, S., Furlan, S. N., Jaeger-Ruckstuhl, C. A., Sarvothama, M., Berger, C., Smythe, K. S., ... & Riddell, S. R. (2021). Immunogenic chemotherapy enhances recruitment of CAR T cells to lung tumors and improves antitumor efficacy when combined with checkpoint blockade. Cancer Cell, 39(2), 193-208.
[20] Rafiq, S., Hackett, C. S., & Brentjens, R. J. (2020). Engineering strategies to overcome the current roadblocks in CAR T cell therapy. Nature reviews Clinical oncology, 17(3), 147-167.
[21] Marofi, F., Motavalli, R., Safonov, V. A., Thangavelu, L., Yumashev, A. V., Alexander, M., ... & Khiavi, F. M. (2021). CAR T cells in solid tumors: challenges and opportunities. Stem cell research & therapy, 12(1), 1-16.
We will respond to you in 1-2 business days.